Uncovering the Spread of Bacteria in Pneumonia

Complete the form below to unlock access to ALL audio articles.
“Prior to this study, it was a mystery how the bacteria escaped from the lungs into the bloodstream,” saidAlan Hauser, MD, PhD, professor in Microbiology-Immunology and Medicine-Infectious Disease. “These findings lay the foundation for future studies to further understand the mechanisms for how the escape to the bloodstream occurs.”
Dr. Hauser and his team used a mouse model of Pseudomonas aeruginosa (PA) pneumonia to examine how the bacterium uses its secretion system to inject a toxin, called ExoS, into cells. ExoS has previously been linked to a higher incidence of infections spreading to the blood.
“If we can understand this at a higher level of detail, perhaps we will be able to design inhibitors that can be flushed into the bloodstream or the lung of a person who has PA pneumonia and block this process. If we can block these processes, we may be able to prevent bacteria from disseminating to the bloodstream during pneumonia,” said Dr. Hauser, also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
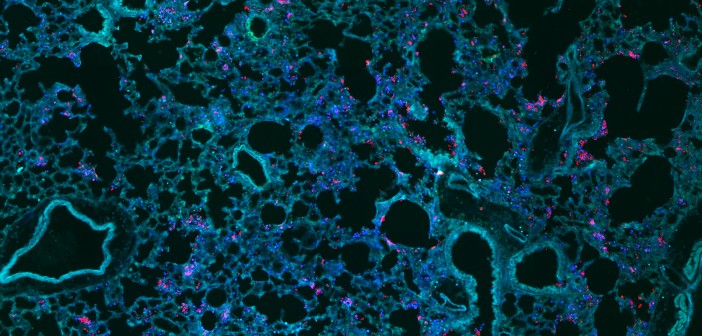
They collaborated with the Center for Advanced Microscopy to use a novel imaging technique to identify cells injected with ExoS. This method allowed them to uncover that ExoS was not only injected into white blood cells, but also epithelial cells that form a barrier between the lung and the bloodstream.
Dr. Hauser also found that injection of the toxin occurred in specific regions which they labeled “fields of cell injection” or FOCI.
“We got a surprising result, that the epithelial cells weren’t randomly being injected, but they were being injected in FOCI within the lungs,” Dr. Hauser said. “Over time, we were able to show as these FOCI became larger and the cells within these injected FOCI began to die.”
Furthermore, they determined that increased FOCI size was associated with enhanced disruption of the barrier between the lungs and bloodstream and ultimately the spreading of the bacteria in to the blood.
“This injection of ExoS results in breakdown of a barrier between the pulmonary space and the vascular space, which allows bacteria to escape from the lungs and to gain access to the bloodstream,” Dr. Hauser said.
Next, Dr. Hauser plans to continue studying the mechanism of how ExoS leads to the formation of FOCI.
“This research might have implications for other bacteria that frequently cause pneumonia and can also escape from the lungs and get into the bloodstream,” he said.



