Developing Novel Cell Therapies by Rewiring T-Cell Genomes
Complete the form below to unlock access to ALL audio articles.
Dr. Theo Roth completed his medical scientist training at the University of California, San Francisco. During this time, Roth developed a novel method that enables the large-scale genomic engineering of primary immune cells without the need for complex viral vectors – non-viral genome targeting. Roth also further refined targeted pooled knock-in screening to rewire immune cell genomes.
In a recent Teach Me in 10 episode, Roth discussed what targeted pooled knock-in screens are, how he is working to accelerate the discovery of cell-based therapies and how this process could reduce the time it takes to transition these therapies from the lab to the clinic.
“What we try to do in the lab is develop new tools that can accelerate the process of discovering new drugs, new medicines for patients,” ‒ Roth.
Cell therapies
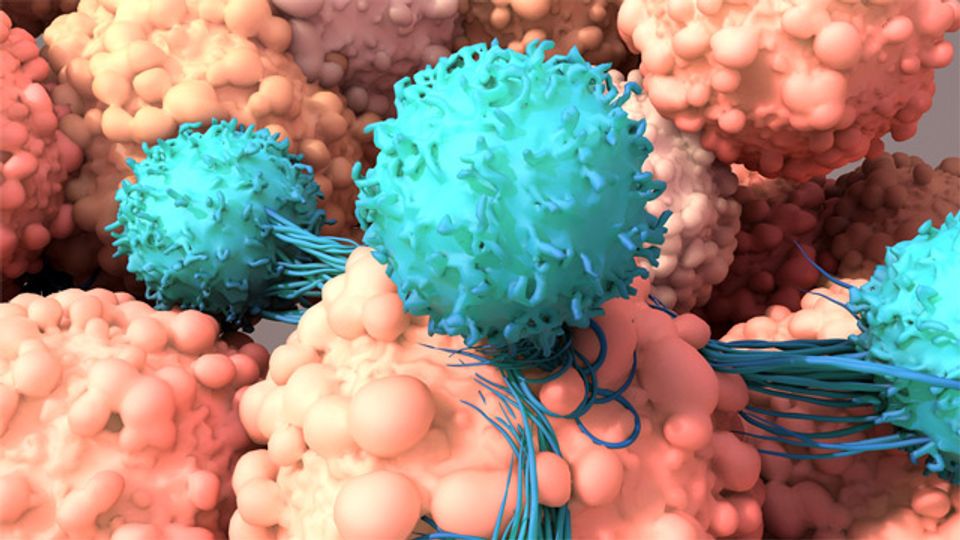
Roth’s research focuses on developing cell therapies, more specifically, modifying the genome of human immune cells to establish if these changes improve their ability to kill cancer cells when they are reintroduced into the patient.
Cell therapy is defined as the introduction of intact live cells into a patient to help lessen or cure a disease. Immune cell therapies for cancer rely on the generation of antigen-specific T cells that can be used to direct an immune attack on a tumor. Despite many clinical successes, there are some limitations to these cell therapies. For example, CAR T cells are not effective against solid tumors, as they often become dysfunctional when faced with the immunosuppressive tumor microenvironment.
To develop cell therapies with increased therapeutic potential, the genomes of the cells can be modified, but testing the effect of inserted modifications can be very time-consuming, (for example, if only one modification is tested at one time) and there is no guarantee that the desired therapeutic outcome will be achieved.
“There’s a huge pipeline of different steps that are required to develop a new drug,” notes Roth. His recent work, which was published in Cell, focuses on the early phases of the drug development pipeline, specifically which type of drug to take forward.
Targeted pooled knock-in screens
The process developed by Roth, targeted pooled knock-in screens, attempts to not only solve the challenge of determining the most promising cell therapy to progress to clinical testing, but can also expedite the testing of various modifications. With pooled knock-in screening, many modifications are made to the genomes of cultured cells ‒ including the introduction of a T-cell receptor that allows the cell to target the cancer cell antigen ‒ and each cell receives a gene that potentially improves cell function. These modified cells make up a cell library, in which every T cell has a different modification. The library can then be used in functional assays to determine the cells’ tumor-killing functionality.
“We start with a healthy human donor. In a therapeutic setting this would be a cancer patient. From that donor we isolate human T cells, which we are able to culture in a dish for about a week or two while we modify those cells to potentially become a therapeutic medicine,” explains Roth. “Instead of testing one cell-based therapy at a time, we can test dozens.”
CRISPR gene editing
As explained by CRISPR Cas9 co-developer and Nobel prize winner Professor Jennifer Doudna, “CRISPR allows scientists to alter the genetic information of any organism including human cells with unprecedented accuracy and efficiency. It is a breakthrough technology that holds huge potential as a strategy to treat and cure diseases, create sustainable biofuels and develop more robust crops.”
Originally discovered as a viral defense system used by bacteria, the CRISPR/Cas9 system is now used for targeted gene editing. Cas9 and guide RNA are used to identify and bind to a specific section of DNA, producing a double-strand DNA break, initiating repair using the new DNA template from the library. This means that during repair, the desired modification is introduced into the DNA.
Roth explains that CRISPR allows for the modification of specific sites within primary immune cell genomes, and is incredibly important as the integration of the new sequences “would only work if we put [the modification] in this one particular site”.
To watch the full Teach Me in 10 video, click here.


