Using Nanoparticle T-Cell Engagers To Treat Acute Myeloid Leukemia
Complete the form below to unlock access to ALL audio articles.
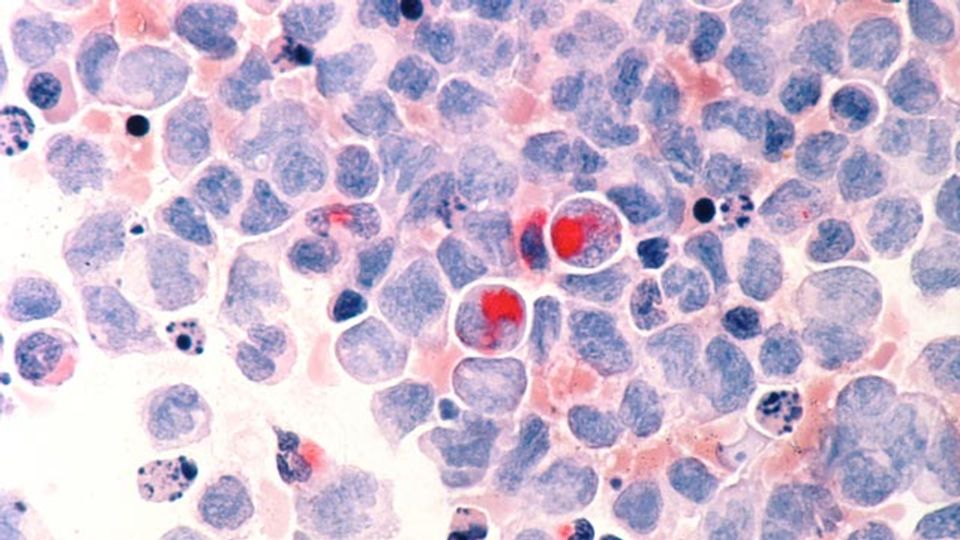
Oncotarget published "Nanoparticle T cell engagers for the treatment of acute myeloid leukemia" which reported that Acute myeloid leukemia (AML) is the most common type of leukemia and has a 5-year survival rate of 25%.
The standard-of-care for AML has not changed in the past few decades. Promising immunotherapy options are being developed for the treatment of AML; yet, these regimens require highly laborious and sophisticated techniques. These authors create nanoTCEs using liposomes conjugated to monoclonal antibodies to enable specific binding. They also recreate the bone marrow niche using our 3D culture system and use immunocompromised mice to enable use of human AML and T cells with nanoTCEs. It is shown that CD33 is ubiquitously present on AML cells. The CD33 nanoTCEs bind preferentially to AML cells compared to Isotype. It's also shown that nanoTCEs effectively activate T cells and induce AML killing in vitro and in vivo. These findings suggest that our nanoTCE technology is a novel and promising immuno-therapy for the treatment of AML and provides a basis for supplemental investigations for the validation of using nanoTCEs in larger animals and patients.
Dr. Abdel Kareem Azab from The Washington University School of Medicine as well as The Washington University McKelvey School of Engineering said, "Acute myeloid leukemia (AML) is the most common type of leukemia; it is characterized by the overproduction of immature myeloid stem cells in the bone marrow and has a 5-year survival rate of around 25%."
The survival curves for AML patients have remained stagnant in the past decades due to the lack of newly approved therapies for AML. However, recent development in novel therapeutics and technologies have shown promising results in preclinical and clinical settings.
TCEs stimulate endogenous T cells and demonstrate high potency and efficacy against tumor cells, circumventing certain limitations of genetically engineering extracted patient T cells to express CARs. This immunotherapeutic option has been shown to be successful for both solid and liquid tumors, but is mostly known for the treatment of hematological malignancies. High CD33 expression has been reported on AML blasts; data show as much as 85–90% of blasts express CD33 in AML patients. Moreover, CD33 expression positively correlates with stage of the disease.
The Azab Research Team concluded in their Oncotarget Research Output, "Our nanoTCE platform uses nanoparticles to create a relatively simple to produce, reproducible, and off-the-shelf solution to overcome the major limitations associated with current immunotherapy techniques such as TCEs and CAR-T cells. Importantly, this technology is highly customizable and provides the flexibility to engage any immune cell for the treatment of the cancer of interest. In this study, we report a CD33/CD3 nanoTCE that targets the CD33 antigen with high specificity using mAbs, which enables a potent and efficacious immunotherapy treatment against AML. Future studies are warranted to investigate this therapy in combination with chemotherapy, the extent this technology eliminates minimal residual disease and relapse, as well as its efficacy in AML patients"
Reference: Alhallak K, Sun J, Muz B. et al. Nanoparticle T cell engagers for the treatment of acute myeloid leukemia. Oncotarget. 2021;2:1878-1885. doi: 10.18632/oncotarget.28054
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source.

