A Non-Invasive Treatment for Difficult-To-Treat Pediatric Brain Cancer
Complete the form below to unlock access to ALL audio articles.
Diffuse intrinsic pontine glioma (DIPG) is a rare pediatric cancer of the brainstem, with a five-year survival rate of 2%. Symptoms develop rapidly due to the fast growth of the tumors and include headaches, problems with balance, eyesight, chewing and swallowing. There is currently no cure for DIPG and the primary therapy presently used is radiotherapy, which can kill the cancerous cells, but produces severe side effects.
ALA sonodynamic therapy (SDT) is a non-invasive treatment method for brain cancer that uses ultrasound energy to produce light in the brain and activate a metabolite of SONALA-001, SonALAsense’s proprietary intravenous formulation of 5-aminolevulinic acid – an amino acid that can cross the blood–brain barrier. In this interview, Technology Networks spoke to Dr. Stuart Marcus, founder and chief medical officer of SonALAsense, to find out how ALA SDT could be a more effective treatment for DIPG and recurrent glioblastoma.
Kate Robinson (KR): Can you tell us about DIPG? Why is this cancer so difficult to diagnose and treat?
Stuart Marcus (SM): DIPG arises from glial cells in an area of the brain stem called the pons and is perhaps the most heinous of the pediatric brain cancers. Rather than grow into a ball shape, like most tumors, DIPG cells grow diffusely around pons cells and actively interfere with them. The pons controls many of the body’s most vital functions, including breathing, blood pressure and heart rate.
DIPG is generally difficult to diagnose because so many nerve functions pass through the pons. As a result, initial symptoms can be vague: double vision, slurred speech, trouble maintaining balance, arm or leg weakness and sometimes headaches.
The treatment challenges are contained in the name: aberrant cells are diffused throughout the pons. Because the pons is essential, it cannot be removed surgically. In addition, current forms of chemotherapy are ineffective. The only current treatment is radiotherapy, which produces severe side effects and poor outcomes. DIPG is an incredibly aggressive cancer, and the median survival is around nine months.
However, when radiotherapy successfully kills DIPG cells, kids can recover some function rapidly. We just need to do a better job of destroying these cancers and preventing them from recurring.
KR: What is sonodynamic therapy (SDT) and how does SDT work with SONALA-001 to treat DIPG?
SM: Sonodynamic therapy is a non-invasive, two-step therapy that delivers a “smart bomb” to brain tumor cells. First, a drug (SONALA-001) is intravenously infused into the patient. The active molecule, aminolevulinic acid (ALA), is a type of amino acid that fast-growing brain tumors accumulate but normal cells mostly ignore. Within a few hours, cancer cells process ALA into a light-sensitive molecule.
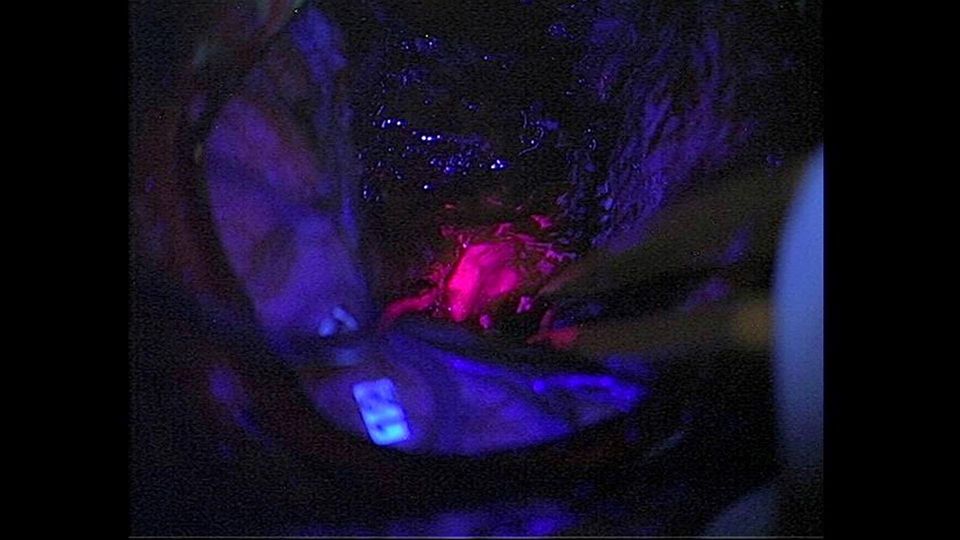
The second step uses MRI-guided focused ultrasound (MRgFUS) to generate light inside tumors, an effect called sonoluminescence. This activates a process similar to photodynamic therapy (which uses light to eliminate skin cancers), selectively killing tumor cells, while leaving normal brain cells intact.
SonALAsense is now recruiting for a trial to examine the safety, pharmacokinetics and preliminary efficacy of sonodynamic therapy using SONALA-001 in combination with the MRgFUS device to treat patients diagnosed with DIPG.
KR: Has SDT shown success with other cancer types in clinical trials?
SM: SDT is being studied to treat recurrent glioblastoma (rGBM), another incredibly deadly cancer, along with other high-grade gliomas. In a phase 0/1 clinical trial, led by neurosurgeon Nader Sanai, MD, of the Ivy Brain Tumor Center at the Barrow Neurological Institute, clinicians delivered SDT to 50% of each tumor. The other half was the control. After four days, the entire tumor was removed.
At the Society for Neuro-Oncology meeting in 2022, Sanai reported that the tumor regions exposed to SDT displayed significantly greater membrane disruption, apoptosis (programmed cell death) and other biomarkers associated with tumor destruction compared to the untreated control. Equally important, patients experienced no dose-limiting toxicities or serious adverse events.
SonALAsense is now conducting a clinical trial at NYU Langone Medical Center, Cleveland Clinic, Mayo Clinic, MD Anderson Cancer Center, UCSF, West Virginia University and the Ivy Brain Tumor Center to establish the optimal combination of SONALA-001 and MRgFUS to treat rGBM.
KR: How does SDT differ from conventional treatments for cancers like high-grade gliomas?
SM: Despite aggressive surgeries and radiotherapy, most GBM patients do not survive more than 18 months. Oncologists have found it virtually impossible to completely eradicate these tumors. As a result, they continuously recur. In addition, surgery and radiotherapy may pose great risks to brain tissue, and patients can lose cognitive and motor function from continued treatments.
By contrast, SDT is non-invasive and only targets tumor cells, leaving healthy brain tissue unscathed. So far, the treatment has been well tolerated.
In addition, ALA has been used for years as a fluorescent marker during surgeries to help delineate tumor from healthy tissue. This experience has shown us that, even when tumors are exposed multiple times to ALA, they never develop an aversion (resistance) to it. This is probably because ALA is a food source and aggressive tumors need to eat.
This is important because GBMs are prone to recur, and patients could conceivably receive multiple treatments to keep their cancers at bay for a long time.
KR: How do you envision SDT will be implemented in clinical settings in the future?
SM: As described above, SDT is completely non-invasive. We envision an outpatient procedure, during which patients receive their SONALA-001 infusion, followed a few hours later by MRgFUS, after which they can then return to their normal activities without fear of interruption from serious side effects.
Dr. Stuart Marcus was speaking to Kate Robinson, Assistant Editor for Technology Networks.


