Treating C. diff Infection and More With Gut Microbiome Transplants
Complete the form below to unlock access to ALL audio articles.
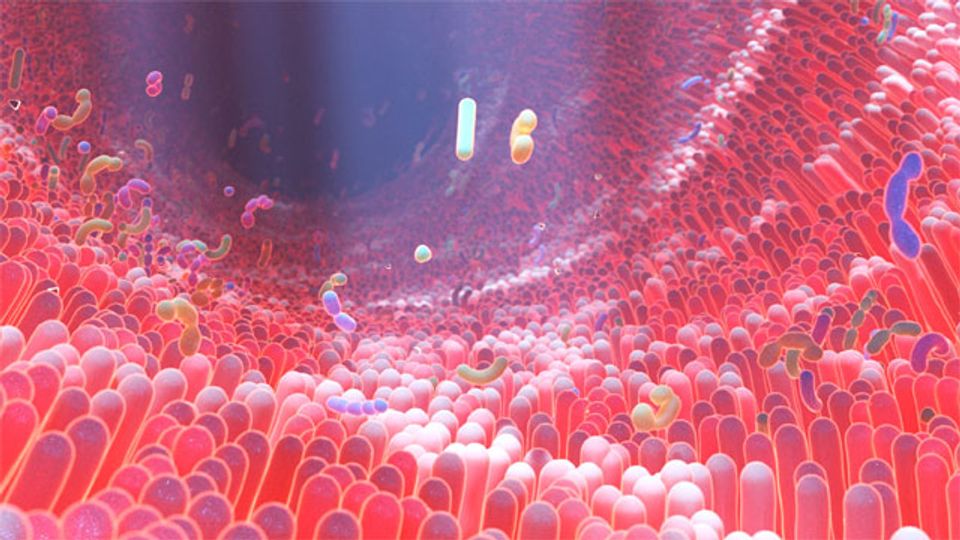
The gut microbiome is composed of billions of microorganisms, spanning hundreds of species. Even between healthy individuals, the microbiomes can vary hugely. These changes can be attributed to lifestyle, genetic or environmental factors and even subtle differences in the composition of the microbiome can make an individual more susceptible to illness.
Clostridium difficile is a bacteria present in the gut, that when it proliferates can produce toxins that cause serious illness. C. diff can be treated using antibiotics, but these can further disrupt the gut microbiome leading to recurrences of C. diff.
Microbiota transplants are regulated by the FDA to treat Clostridium difficile infection but can be time-consuming and arduous for both clinicians and patients. We spoke to Dr. Thomas Lendvay, CMO and co-founder of Tend, about their new device that could make microbiota transplants easier and more accessible and could pave the way to using transplants to treat more than C. diff infection.
Katie Brighton (KB): First of all, could you highlight the role of the gut microbiome in health and disease?
Thomas Lendvay (TL): Most people would be surprised to know that people are made up of more microbes than human cells by a pretty big margin. All those microbes influence important things for our health like digestion, inflammation, metabolism, immunity and brain function. And when our microbiome gets out of balance or is dominated by a few community members, things can go the other way and we end up with poor digestion, flares of inflammation, altered immune defenses and even mental health changes. Our gut microbiome is this superpower we all have that we are just beginning to fully understand in terms of its potential for health and healing.
KB: How does the microbiome become disrupted and what happens when it does?
TL: Diet can alter the gut microbiome, but the most dramatic disruptors are things like antibiotics and some chemotherapies which act sort of like atomic bombs for our microbes. These two offenders, albeit necessary for many reasons, create significant collateral damage within our guts. They usually wipe out many families of microbes which typically work together with other families to do the “work” of our gut function. When you remove some of the family members in the community, the community becomes disorganized and doesn’t function as well.
For example, once you change this balance, some of the microbes that existed in a certain quantity before can now overgrow and create chaos. That’s what happens with C. diff, a potentially deadly disease that affects many people each year. Antibiotics and chemotherapies wipe out large swathes of microbe families and allow space for these bacteria to overgrow and release toxins that make people seriously ill, in some cases leading to bacteria in the bloodstream and ultimately sepsis.
KB: Why are antibiotics not very effective at treating gut infections such as recurrent C. diff infection?
TL: Ironically, the first- and second-line treatments for Clostridium difficile infections are antibiotics that, while they can irradicate C. diff in some instances, can also create further disruptions by killing off more bacteria. Up to 40% of C. diff patients can recur. Patients experience severely debilitating diarrhea, abdominal pain and often cannot absorb nutrients well so lose a lot of weight.
KB: What is a fecal microbiota transplant? How is it performed?
TL: A fecal microbiome transplant (FMT), also known as a gut microbiome transplant, is the transfer of stool that contains the gut microbiome from one person to another, or from the same person back into themselves. The former is the most common version of gut microbiome transplant where a “healthy” donor donates a sample for use in an ill patient with a poor gut microbiome. The donor is thoroughly screened for pathogens like viruses and bacteria that may harbor antibiotic resistance blueprints. In the US, the FDA regulates the use of microbiome transplants in C. diff patients. Beyond this use case, special permission from the FDA is required. Just like in other types of organ transplants, some grafts “take” and others don’t.
A person providing a stool sample to help repopulate their own microbiome after antibiotic treatment or chemotherapy is far less common and only performed under clinical trials. The patients who have undergone this process, called “autologous” or self-derived microbiome transplant, have been in studies of very ill patients who are undergoing bone marrow transplants and who have a known period of time where it is expected that they will be on disruptive antibiotics or chemotherapies. In this instance, the microbiome transplant is like poop insurance for when they need to replenish what they originally had.
Microbiome transplants are carried out in various ways. The predominant method in the US is by colonoscopy where a solution of the donor’s stool, usually after mixing with saline, filtering and adding preservatives to protect during the freezing storage, is instilled into the colon of the patient through the scope. Other methods of microbiome transplant administration are through enemas, or tubes placed down the esophagus and either into the stomach or beyond.
An emerging route of administration, and supported by evidence from research of its efficacy, is the use of orally ingestible capsules of prepared microbiome transplant solutions. These capsules tend to be delayed-release or acid resistant so they don’t open until after they’ve cleared the stomach. It may sound strange to ingest capsules of the microbiome, but it’s far less invasive than colonoscopy. Many patients prefer an oral route to a rectal route which, in the case of colonoscopy, requires sedation or anesthesia and in very ill patients can involve a higher risk for complications.
KB: What challenges are associated with a gut microbiota transplant?
TL: One of the major challenges to microbiome transplants is the effort required and lack of standardization in the processing of the stool samples. The user experience for the clinicians or researchers and their teams is arduous. Since many transplant administration routes are invasive – tubes down your throat or scopes from below – the patient experience is also unfavorable. There are centers that do the processing but because the labor required and the mess incurred is substantial, many hospitals and clinicians who see patients who need microbiome transplants cannot provide one. This creates an access bottleneck for patients in need.
KB: Tend has developed the Gut Microbiome Collect and Prep (CAP) device to improve fecal microbiota transplants, could you tell us a little more about how it works?
TL: Our CAP device allows clinicians to use a single device to collect, filter, mix, homogenize and encapsulate gut microbiome material in stool. The resulting capsules can then be frozen and stored for later patient use. Clinicians have reported that using our CAP device cuts 90% of prep time from their current method. Furthermore, our method doesn’t require dilution with saline, which means less processing that may damage some of the bacteria, compared to other methods. The device is smaller than a toaster and is manually driven making it very portable and inexpensive relative to the labor required to do the conventional mixing. We also are coupling the DNA or blueprint data about the donor’s microbiome with the results from the recipients’ microbiomes before and after FMT to learn if there are signatures of the donor or the patient that work better. For example, when you transplant a kidney, you have to make sure there is a good “match” between the donor and the recipient. It’s possible that the same matching applies to whether a microbiome transplant will work better than others. Does the donor have a microbiome that aligns particularly well with a recipient? We aim to find out.
KB: Massachusetts General Hospital has initiated a clinical study validating the CAP device as an encapsulation method for FMT. If the trial is successful, how do you see the CAP device being used in the future? Are there applications outside of FMT?
TL: If the Mass General study shows that patients who had capsules prepared with our device are cured of their C. diff infections and that the device made the workflows of sample processing much easier, we envision that also other sites will adopt this method for processing. The more that happens, the more standardization will come to the field, allowing for studies using microbiome transplants to be more easily and reliably compared to one another, potentially accelerating adoption and increasing access to this superpower for healing.
The question about other applications is one I am also really excited about. Increasing access to microbiome transplants for patients with C. diff is a major upside to our technology. It’s possible that as more are performed, coupled with the growing concerns about overuse of antibiotics, microbiome transplants may become the first-line therapy for C.diff.
In addition to C diff, there are a host of other health conditions, affecting millions of people, which may benefit from microbiome transplants. Trials are underway already on many different health conditions with promising signals. For example, there are a number of studies looking at how microbiome transplants can help patients suffering from inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease.
Another gut ailment that millions of Americans suffer from is irritable bowel syndrome (or IBS) which isn’t one particular disease as much as it is a collection of symptoms like chronic diarrhea, constipation, bloating, abdominal pain and cramps that cause many to avoid social gatherings or map out where bathrooms are at any public venue in case there is an urgent need. Researchers are exploring whether microbiome transplants can help rebalance the gut of patients suffering from IBS.
Outside of intestinal diseases, there have been some remarkable research findings on the use of microbiome transplants for patients with metastatic cancers who don’t respond to immunotherapy to help the patient fight the cancer. This implies that the superpower of the microbiome may change how a patient’s immune system functions and reacts to cancers. Then there are the mental and behavioral health disorders that researchers are looking to investigate such as the role of transplants in improving depression, bipolar disorder and even autism. This is based on the premise of the “gut–brain axis” which is the communication from the gut to the brain and back. Several chemicals that are primarily active in the brain and drive our moods are produced in the intestines and by the gut microbiome.
Finally, getting back to my previous example of poop insurance, there is a possibility that our technology could someday be used to help “bank” a healthy person’s microbiome in anticipation of some disruptive event like taking a course of antibiotics, undergoing chemotherapy or travel to regions where dysentery rates can be high. One could replenish their own microbiome when the microbiome becomes out of balance after such events. This is an example of an autologous microbiome transplant and although the opportunities are large, this will require highly rigorous studying to make sure it’s safe and effective.
At Tend, we believe that in the next 5–10 years clinicians will be looking at many common diseases through the lens of our gut microbiome. Therapies can then be directed at manipulating the microbiome through natural microbiome transplants.
Thomas Lendvay was speaking to Katie Brighton, Scientific Copywriter for Technology Networks.


