First Entirely 3D-printed Organ-on-a-Chip with Integrated Sensors

Complete the form below to unlock access to ALL audio articles.
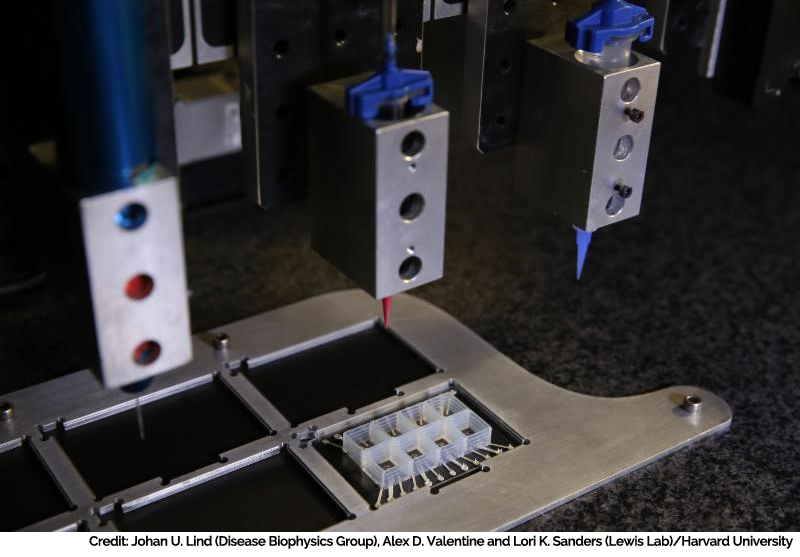
The heart-on-a-chip is made entirely using multi-material 3D printing in a single automated procedure, integrating six custom printing inks at micrometer resolution. Credit: Credit: Lori K. Sanders and Alex D. Valentine/Lewis Lab
Researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University and the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) have made the first entirely 3D-printed organ-on-a-chip with integrated sensing. Built by a fully automated, digital manufacturing procedure, the 3D-printed heart-on-a-chip can be quickly fabricated with customizable size, shape and other physical properties, allowing researchers reliable date to be easily collected for short-term and long-term studies. The study is published in Nature Materials.
"This new programmable approach to building organs-on-chips not only allows us to easily change and customize the design of the system by integrating sensing but also drastically simplifies data acquisition," said Johan Ulrik Lind, Ph.D., first author of the paper and postdoctoral fellow at SEAS and the Wyss Institute.
In this video, learn how Wyss Institute and Harvard SEAS researchers have created a 3D-printed heart-on-a-chip that could lead to new customizable devices for short-term and long-term in vitro testing. Credit: Johan U. Lind (Disease Biophysics Group), Alex D. Valentine and Lori K. Sanders (Lewis Lab)/Harvard University
3D Printed Heart-on-a-Chip from Wyss Institute on Vimeo.
"Our microfabrication approach opens new avenues for in vitro tissue engineering, toxicology and drug screening research," said Kit Parker, Ph.D., senior coauthor of the study, who is a Wyss Core Faculty member and Tarr Family Professor of Bioengineering and Applied Physics at SEAS.
Organs-on-chips mimic the structure and function of native tissue and have emerged as a promising alternative to traditional animal testing. Wyss Institute research teams led by Parker and Wyss Founding Director and Core Faculty member Donald Ingber, M.D., Ph.D., have developed microphysiological systems that mimic the microarchitecture and functions of lungs, hearts, tongues and intestines.
However, the fabrication and data collection process for organs-on-chips is expensive and laborious. Currently, these devices are built in clean rooms using a complex, multi-step lithographic process and collecting data requires microscopy or high-speed cameras.
"Our approach was to address these two challenges simultaneously via digital manufacturing," said Travis Busbee, coauthor of the paper and graduate student at Wyss and SEAS. "By developing new printable inks for multi-material 3D printing, we were able to automate the fabrication process while increasing the complexity of the devices."
The researchers developed six different inks that integrated soft strain sensors within the microarchitecture of the tissue. In a single, continuous procedure, the team 3D printed those materials into a cardiac microphysiological device - a heart on a chip - with integrated sensors.
"We are pushing the boundaries of three-dimensional printing by developing and integrating multiple functional materials within printed devices," said Jennifer Lewis, Sc.D., who is a Wyss Core Faculty member and the Hansjorg Wyss Professor of Biologically Inspired Engineering at SEAS, and senior coauthor of the study. "This study is a powerful demonstration of how our platform can be used to create fully functional, instrumented chips for drug screening and disease modeling."
The chip contains multiple wells, each with separate tissues and integrated sensors, allowing researchers to study many engineered cardiac tissues at once. To demonstrate the efficacy of the device, the team performed drug studies and longer-term studies of gradual changes in the contractile stress of engineered cardiac tissues, which can occur over the course of several weeks.
"Researchers are often left working in the dark when it comes to gradual changes that occur during cardiac tissue development and maturation because there has been a lack of easy, non-invasive ways to measure the tissue functional performance," said Lind. "These integrated sensors allow researchers to continuously collect data while tissues mature and improve their contractility. Similarly, they will enable studies of gradual effects of chronic exposure to toxins."
"Translating microphysiological devices into truly valuable platforms for studying human health and disease requires that we address both data acquisition and manufacturing of our devices," said Parker. "This work offers new potential solutions to both of these central challenges."

