Promising Targeted Drug Identified for Rare Leukemia
Complete the form below to unlock access to ALL audio articles.
Targeted drugs have been developed to supplement chemotherapy in the treatment of cancer. These drugs only affect cancer cells, leaving healthy cells alone. Venetoclax is a new targeted therapy option for the treatment of acute myeloid leukemia (AML). Venetoclax was recently granted marketing authorisation in Finland.
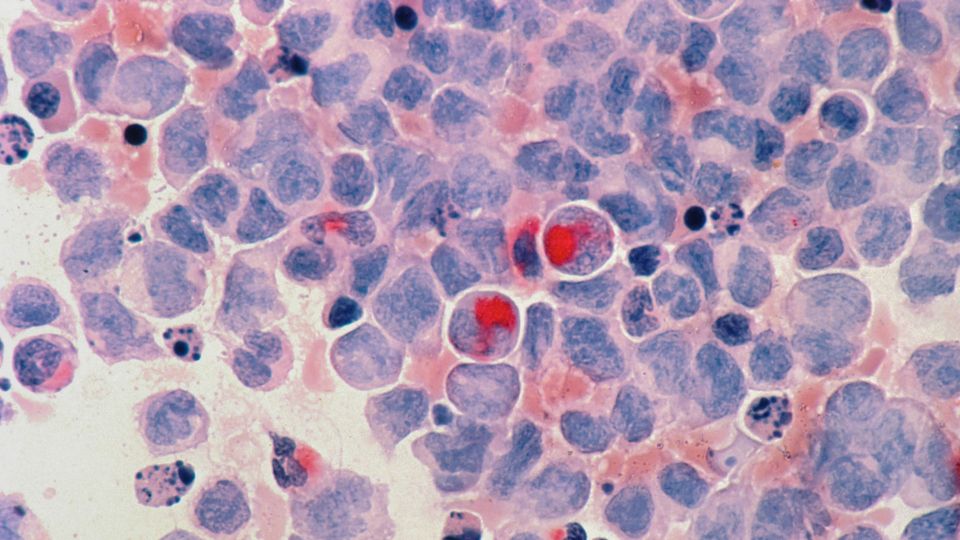
Venetoclax works by sensitising cancer cells to programmed cell death. However, a new study now shows that venetoclax does not appear to be effective against erythroid and megakaryoblastic leukemias, two rare subtypes of the disease that are difficult to treat. In these leukemia types, malignant cells resemble blood stem cells that produce red blood cells or platelets. Currently, few treatment options are available to these patients.
The study carried out by the University of Helsinki, HUS Comprehensive Cancer Center and the University of Copenhagen identified a new targeted drug, which may in the future offer a therapeutic option to patients with these subtypes of the disease. The study was published in the Blood journal in December.
Further research needed
In the laboratory, the researchers screened a wide selection of pharmaceutical agents that could be effective specifically against erythroid or megakaryoblastic leukemia cells.
Want more breaking news?
Subscribe to Technology Networks’ daily newsletter, delivering breaking science news straight to your inbox every day.
Subscribe for FREE“The introduction of venetoclax has significantly improved the prognosis of AML patients. However, our research indicates that venetoclax is unlikely to function optimally against the subtypes of AML in our focus. Nevertheless, the finding should be verified in larger patient datasets,” says physician-scientist Olli Dufva.
Potential to improve prognosis
AML is the most common type of acute leukemia in adults. It can be divided into subtypes based on mutations and the degree of differentiation of leukemia cells. One challenge associated with the use of targeted drugs is identifying patients who benefit from the new drug options. This study contributes to making the selection of targeted drugs more precise.
“The laboratory findings provide evidence that patients with erythroid or megakaryoblastic acute leukemia would be a promising group for investigating the efficacy of BCL-XL inhibitors in clinical use,” says postdoctoral researcher Heikki Kuusanmäki.
The researchers believe that BCL-XL inhibitors will be trialled in the treatment of these leukemia types in the near future.
“This finding may in the future improve the prognosis of these very rare and difficult-to-treat leukemias,” says Professor of Translational Haematology Satu Mustjoki from the University of Helsinki and HUS Comprehensive Cancer Center.
Reference: Kuusanmäki H, Dufva O, Vähä-Koskela M, et al. Erythroid/megakaryocytic differentiation confers BCL-XL dependency and venetoclax resistance in acute myeloid leukemia. Blood. 2022:blood.2021011094. doi: 10.1182/blood.2021011094
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source.

