Gene Regulators Work Collaboratively To Determine Schizophrenia Risk
Complete the form below to unlock access to ALL audio articles.
Schizophrenia is a complex mental health disorder that affects approximately one percent of the global population.
Symptoms of the disorder are typically classified into two groups: "positive" symptoms, such as hallucinations, delusions and repetitive moments that are difficult to control, and "negative" symptoms, such as the loss of ability to display emotion, apathy, difficulty speaking and withdrawal from social situations. A third sub-group of symptoms, often referred to as cognitive symptoms, include impairments of an individual's ability to think, such as disorganized thoughts, memory issues and inability to focus.
Despite more than a century of research, the pursuit to untangle the neurobiology of schizophrenia has been largely unsuccessful, a failure attributed to the heterogenic nature of the disorder.1
One area of focus for scientists has been a potential genetic component of schizophrenia. Previous studies have demonstrated that the risk of illness is approximately 10% for a first degree relative, and 3% for a second-degree relative.2 What's more, in twin studies, the risk of one twin having schizophrenia in monozygotic twins is 47% if the other twin has the disorder, whereas in dizygotic twins the risk is just 12%.
The advent of genome wide association studies (GWAS) in genomics has facilitated research in the schizophrenia field, revealing at least 143 chromosomal sites that are associated with a risk for schizophrenia.
What is a GWAS study? In genetics research, a GWAS study is an observational analysis of a genome-wide set of genetic variants across a population. The aim of the study is to identify whether any specific variants are associated with a certain trait, or phenotype, such as a disease. The most commonly occurring variants are single-nucleotide polymorphisms (SNPs), which involve a single letter change in the DNA code.
Individually, however, these sites can only account for a small fraction of the genetic risk.
And so, researchers from the Icahn School of Medicine at Mount Sinai, led by Kristen Brennand, have dug deeper into the mystery of schizophrenia's genetic component. In a new study published in Nature Genetics, they explore the potential role of expression quantitative trait loci, or eQTLs, that govern the expression of several genes in schizophrenia.3 Interestingly, >40% of the chromosomal sites implicated in schizophrenia contain these regulators.
Exploring eQTLs with the power of stem cells
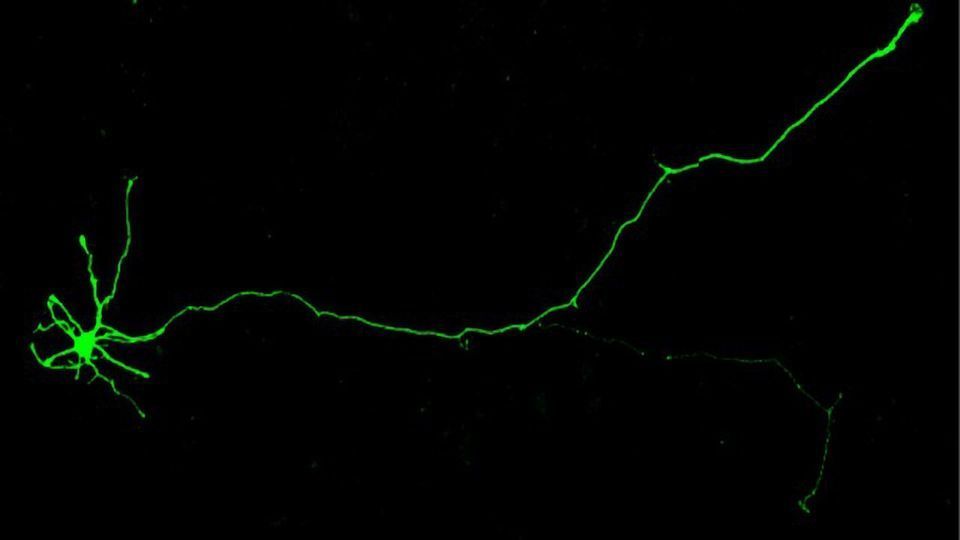
Brennand and colleagues harnessed advances in stem cell research to explore the role of eQTLs. They created neurons from isogenic human induced pluripotent stem cells, a method which enables scientists to grow an individual's unique neuronal cells in a petri dish from stem cells taken from their skin.
Using the gene-editing tool CRISPR, the research group mimicked the interaction of multiple risk genes suggested by the literature to contribute to schizophrenia. They explored the downstream molecular consequences of increasing or decreasing expression of four schizophrenia-implicated genes: FURIN, SNAP91, TSNARE1 and CLCN3 – all of which harbour eQTLs. To initiate changes towards the direction predicted to heighten the risk for schizophrenia, expression was increased for three of the genes, and decreased for one.
Gene regulators work together
Manipulating the expression of the four genes was found to subsequently alter the expression of a further 1,261 other genes. Of these genes, 665 were increased in expression, and 596 decreased. The authors note that this is "many more than would be expected if the genes had been merely acting individually", thereby implying a "synergistic" mechanism – i.e., the gene expression regulators are potentially working together to increase an individual's risk of schizophrenia.
Interestingly, a large proportion of the genes affected downstream contained variants that have been previously linked to autism spectrum disorder (ASD) and bipolar disorder in addition to schizophrenia.
"This unexpected synergy between gene variants demonstrated how even subtle genetic variations can impact neuronal function," said Brennand. "These interactions emphasize the importance of considering the complex nature of schizophrenia and other psychiatric disorders, where a combination of gene variants contributes to disease."
The induced gene expression changes also mirrored those observed in postmortem brains of individuals with ASD, bipolar and schizophrenia.
In induced pluripotent stem cell neurons derived from individuals with childhood-onset schizophrenia (a rarer form of the disorder believed to be more genetic in origin), the same downstream gene expression changes were noted.
"Individually, these gene regulators have a modest effect on the brain. Working in concert, they exert different and more significant effects on the brain – effects that boost schizophrenia risk," explained David Panchision, chief of the Developmental Neurobiology Program at the National Institute of Mental Health. "Learning more about the downstream cellular and molecular effects of such synergy holds hope for advances in precision psychiatry and more personalized medicine."
Future directions
The authors identified that the gene changes observed largely result in a loss-of-brain function when screened individually in a zebrafish model. Subsequently, they emphasize the need for further exploration of these genes with regards to the pathophysiology of schizophrenia. "There is an overwhelming need for future studies to similarly model such multi-gene interactions in complex cells and circuits," concluded Brennand.
References:
1. Patel et al. 2014. Schizophrenia: Overview and Treatment Options. Pharmacy and Therapeutics. PMID: 25210417.
2. McDonald and Murphy. 2003. The new genetics of schizophrenia. The Psychiatry Clinics of North America. PMID: 12683259.
3. Schrode et al. 2019. Synergistic effects of common schizophrenia risk variants. Nature Genetics. DOI: https://doi.org/10.1038/s41588-019-0497-5.


