Antigen vs Antibody – What Are the Differences?

Complete the form below to unlock access to ALL audio articles.
Antigen vs antibody: the basics
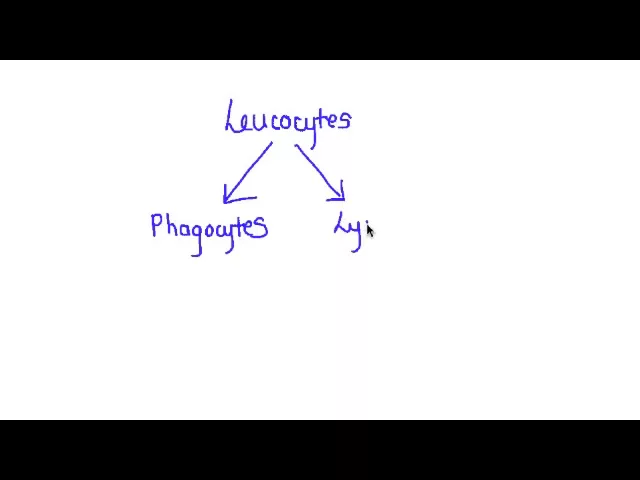
An antigen is any substance that prompts your body to trigger an immune response against it. Antigens include allergens, bacteria and viruses. Antibodies are Y-shaped proteins that the body produces when it detects antigens. Antibodies are produced by immune cells called B cells.
Antigens are molecules capable of stimulating an immune response. Each antigen has distinct surface features, or epitopes, resulting in specific responses.
Antibodies (immunoglobins) are Y-shaped proteins produced by B cells of the immune system in response to exposure to antigens. Each antibody contains a paratope that recognizes a specific epitope on an antigen, acting like a lock and key binding mechanism. This binding helps to eliminate antigens from the body, either by direct neutralization or by ‘tagging’ for other arms of the immune system.
Comparison Chart on Differences Between Antigen & Antibody
Antigen | Antibody | |
Overview | Substance that can induce an immune response | Proteins that recognize and bind to antigens |
Molecule type | Usually proteins, may also be polysaccharides, lipids or nucleic acids | Proteins |
| Origin | Within the body or externally | Within the body |
Specific binding site | Epitope | Paratope |
Image |
|
|
Utilizing Antibodies and Antigens in Diagnostics
When infected with a pathogen such as SARS-CoV-2, the body produces antibodies that bind specifically to the antigens to help eliminate the pathogen. This binding can be harnessed to develop antibody and antigen-based diagnostic tests.
An antibody test reveals if a person has already been exposed to an infection, by detecting antibodies in their blood or serum. This can be done by a laboratory-based test such as an ELISA (Enzyme-Linked Immunosorbent Assay) or CIA (chemiluminescent immunoassay), or a point-of-care test based on lateral flow technology.
Antibody tests are not usually used to diagnose current infection as it takes the body some time to produce antibodies. During the period before the adaptive immune system kicks in, the fast-acting and non-specific innate immune response combats infection. A negative test result may occur if the test is taken too soon after infection before antibodies have been produced by the body. False positive test results could also occur due to cross-reactivity.
Antibody tests are useful to help track the spread of a disease, identify those who should be prioritized for vaccinations, and highlight potential donors for convalescent plasma therapy.
Unlike nucleic acid-based tests such as PCR, which detect the presence of genetic material, antigen tests detect proteins, such as those found on the surface of a virus. Accuracy can be a problem, with antigen tests typically having a much lower sensitivity than PCR. However, they usually provide test results rapidly, are relatively cheap, and can be more amenable to point-of-care use, which could make them more suitable for testing in the community and in remote regions.
The role of antigens and antibodies in vaccinations
Vaccines contain antigens that stimulate the B lymphocytes of the immune system to respond by producing plasma cells which secrete disease-specific antibodies (Primary response). Some of the B cells become memory B cells, which will recognize future exposure to the disease. This results in faster and more intense production of antibodies, which effectively work to eliminate the disease by binding to the antigens (Secondary response).
Types of therapeutic antibodies include:
- Immunoglobulins
- Antibody fragments
- Antibody-drug conjugates
- Bi-specific antibodies
- Radioimmunoconjugates






