“Common Cold” Coronaviruses Could Help Produce Anti-SARS-CoV-2 Immune Cells
Complete the form below to unlock access to ALL audio articles.
Researchers examining immune cells produced against coronaviruses have uncovered a wealth of information about how this critical aspect of immunity could fight off COVID-19, the disease caused by the novel coronavirus SARS-CoV-2. The new study provides hope that some immune responses to SARS-CoV-2 could be long-lasting.
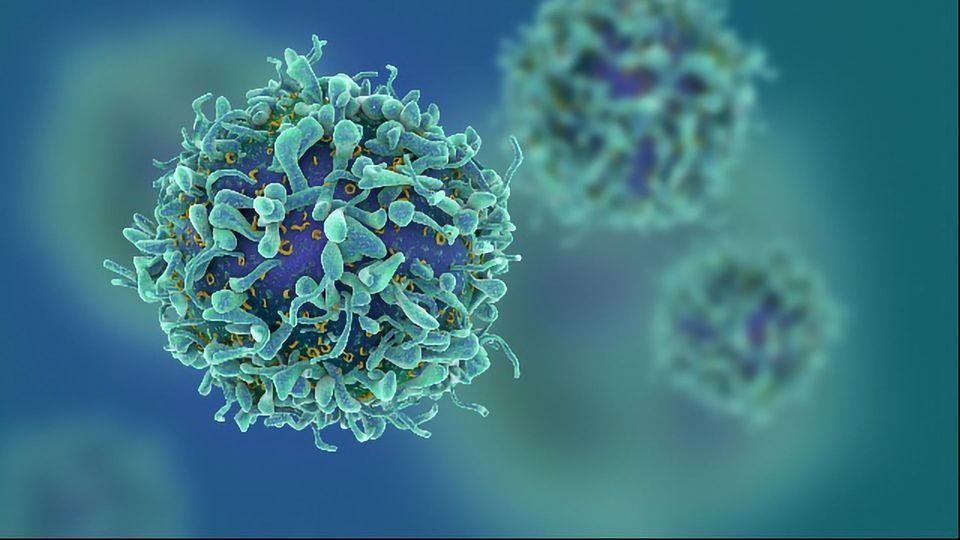
The study, published in Nature by the lab of Antonio Bertoletti at the Duke-NUS Medical School, trawled through a trove of data on how T cells, a key component of viral immunity, respond to infection by SARS-CoV-2. The Singapore-based team also had valuable access to patients who were infected by the related SARS-CoV virus (the cause of SARS) in 2003. Finally, they identified that some people who had no exposure to either SARS-CoV-2 or SARS-CoV still harbored T cells that could react to regions of SARS-CoV-2. The exact reason for the presence of these T cells is still unknown, but authors suspect it could have resulted from infection with coronaviruses known to cause the “common cold” in humans or other, still-unknown coronaviruses. Whether the presence of these cells confers protection against COVID-19 is still unclear.
“This is among the first publications to closely map the parts of the virus targeted by T cells. In doing so, the team have looked at the virus beyond just the spike that people often focus on,” said Daniel Altmann, professor of immunology, Imperial College London, who was not involved in the study.
A family of viruses
SARS-CoV-2 belongs to a family of viruses called Coronaviridae. There are six other viruses in the family known to affect humans. Four of them cause the common cold (this can also be triggered by other, unrelated viruses, such as rhinoviruses), one causes SARS and one MERS. As research into SARS-CoV-2 is so novel, studying the other viruses in the Coronaviridae family could provide insight into how to beat this relative newcomer.
Once the body’s immune system has fought off an infection, a tiny number of immune cells hang around, like dedicated fans who follow a band long after their last good record came out. These memory cells are ready and waiting for any signs of their matched virus to re-emerge. At this point, they undergo a rapid process called “clonal expansion”, where they multiply in number so as to produce a response far greater and more impactful than was seen upon first infection. Keeping with musical analogies, this would be the equivalent of Bob Dylan hitting the Billboard No.1 for the first time at age 78 (which actually did happen earlier this year).
But SARS-CoV-2 is still poorly understood, and Bertoletti’s team wanted to investigate whether T cells against this virus would also hang around.
Firstly, the team looked at SARS-CoV-2-specific T cells in patients who had recovered from COVID-19. Looking at blood samples from 36 individuals, the team examined whether the T cells present in their blood would react to the presence of selected subunits of SARS-CoV-2. In nearly all the individuals studied, responses were seen to multiple regions of the protein. Interestingly, the team noted that some patients had T cells that reacted to regions also targeted by SARS-recovered individuals.
This prompted the team to look in more detail at people who had recovered from SARS. How long lasting was their immunity? Nearly 20 years after that epidemic swept East Asia, Bertoletti’s team discovered that reactive cells still circulated inside the bloodstream of people who had beaten off the virus. These superfan cells were also able to react to SARS-CoV-2 peptides.
No infection doesn’t mean no immune response
The presence of these long-lasting memory cells in SARS survivors bodes well for COVID-19, says Bertoletti. “Long-lasting T cell immunity is likely to be present also in COVID-19,” he says.
Finally, the team looked at people who had not been exposed to either SARS-CoV or SARS-CoV-2. Remarkably, 19 out of 37 unexposed people had T cells that could respond to SARS-CoV-2 peptides, although the peptides that these cells reacted to were different to those that SARS survivors’ T cells reacted to.
Further analysis of the peptides that stimulated uninfected people’s T cells produced a strange finding: they weren’t present in any known coronavirus other than SARS-CoV-2 or SARS-CoV. The authors suggest that infection by yet-to-be-discovered coronaviruses may have produced these T cells, although more research will be needed to work out exactly what these cells were doing there.
It’s important to consider that the presence of T cells that can react to a peptide of SARS-CoV-2 in a person’s bloodstream doesn’t necessarily mean that they are protected against COVID-19. What Bertoletti’s paper does point out is that the T cells found in uninfected people’s bloodstreams were more likely to react to the first-produced SARS-CoV-2 proteins. If these proteins can be disrupted by T cell responses, any subsequent infection might be limited in its ability to harm. “Memory T and B cells will not likely be able to completely avoid a re-infection, but they will effectively contain the infection, stopping the spread of the virus. What I am saying is, if we turn SARS-CoV-2 infection to a normal cold, wouldn’t [that] be nice?” says Bertoletti.
Lessons from pandemics past
Furthermore, lessons learned from other viral outbreaks, H1N1 influenza pandemic of 2009, could be instructive. In a review published in Nature Reviews Immunology, authors Alessandro Sette and Shane Crotty pointed out evidence that pre-existing T cell immunity to H1N1 presumably resulted in the 2009 outbreak’s V-shaped age distribution, where older people often fared better than younger adults after infection. Answering the question of whether pre-existing immunity helps protect against COVID-19 remains an important research goal.
What do these results mean for people who have recovered from COVID-19 and want to prove they are immune? The initially popular idea of an “immunity passport” that allowed such individuals to resume pre-pandemic habits has been roundly dismissed by experts. Bertoletti says that any future assessments of whether individuals are protected against the virus will require researchers to better understand the contribution of antibodies and T cells to fighting off the virus. “We still don’t have real “correlate of protection”. In most of viral infections the antibody and T cells act in coordination,” Bertoletti states.
The need to consider both types of immunity applies to testing as well, “Antibody [tests] might underestimate the number of infected,” says Bertoletti. “But it is easier to test the presence of antibodies than T cells. It could be nice to test both.”


