Gut Microbiome Changes Identified After Spinal Cord Injury
Complete the form below to unlock access to ALL audio articles.
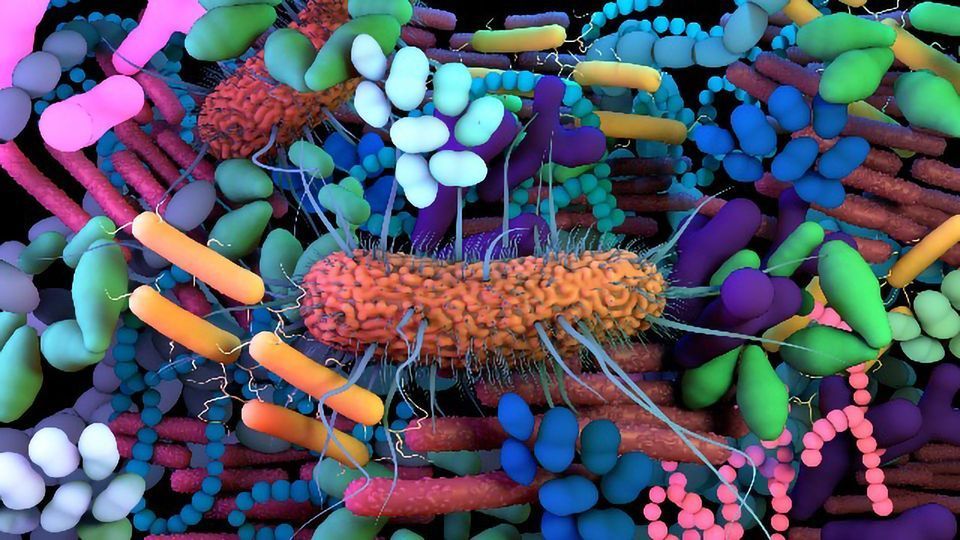
Over recent decades, there has been a dramatic increase in the amount of research exploring the human microbiome – the community of microbes that call our body home. Microbes, including bacteria, bacteriophage, fungi and protozoa, are known to play an integral role in human health. Research is also demonstrating that dysregulation of the microbiome can contribute to – and be a consequence of – various diseases.
Spinal cord injury (SCI) refers to damage of the spinal cord that can temporarily or permanently inhibit its function. Depending on the nature of the injury, SCIs can be extremely challenging to treat due to the varying systemic and neurological outcomes.
A pilot study led by Professor Phillip Popovich has placed focus on how traumatic SCI might impact the gut microbiome – the population of microbes inhabiting the digestive tract. Specifically, the work has utilized a metagenomics approach: a high-throughput method that analyzes all microbe populations in a sample, providing genetic, physiological and biochemical data.
While this is a novel strategy, with the findings based on mammalian models of traumatic SCI, the authors are confident that the research provides a step towards understanding how gut dysbiosis might impact a patient's outcome after SCI.
In this interview, Technology Networks spoke with Ahmed Zayed, a postdoc in the Sullivan laboratory at The Ohio State University and co-author of the study to learn about the key findings and what implications they could have for the SCI research field.
Molly Campbell (MC): Can you discuss what gut dysbiosis is, and the emerging data that suggests it may contribute to human diseases, particularly SCI?
Ahmed Zayed (AZ): Gut dysbiosis is a shift in the composition of the gut microbiome (that includes microbes, viruses and fungi) to a new, persistent and imbalanced state. This is problematic because the functions (or metabolic activities) served by these microorganisms get disrupted, resulting in several documented human disorders, including immune dysfunction and several metabolic diseases that are also caused by SCI. This “concerted action” from the injury and the microbiome, including a positive feedback loop from the gut--spinal cord-brain axis, can exacerbate the condition of people suffering from a SCI.
MC: Can you distinguish between 16S rRNA amplicon sequencing and genome- and gene-resolved metagenomic analyses? Why is the latter a preferred option for novel research?
AZ: In our study, we chose to use gene- and genome-resolved metagenomics instead of 16S rRNA amplicon sequencing. The 16S rRNA technique depends on making numerous assumptions about the microorganisms that carry them. That is because it only focuses on short stretches of the microbial sequences (only hundreds of bases) to infer “who is there”. However, this technique fails to capture “what is being done by these microbes” since there is no sequence information about the genes that are carried by these microbes. Additionally, viruses do not carry 16S rRNA genes, and hence this technique is completely blind to viruses. Metagenomics provides enough resolution to investigate the microbial functions and viruses, and we do so in a lineage-by-lineage framework that allows us to highlight the important lineages and the functions that they serve. Many of these lineages can be new to science and are not part of the available “reference databases”.
MC: You found that, after SCI, the number of "beneficial" bacterium decreased. Firstly, what makes a bacterium "beneficial", and secondly, how did you measure these decreases?
AZ: Beneficial bacteria provide a health benefit to their hosts. For example, many microbes in our gut provide us with vitamins and other metabolites that can be of great benefit to both the immediate gut environment and to distal places such as the brain and the spinal cord. In our study, we found new microbial species, that were capable of making important metabolites (such as tryptophan and vitamin B6) that both support the integrity and motility of the gut and are required for the biosynthesis of neuroactive compounds essential for the health of our central nervous system. We tracked the relative abundance of these microbes, by quantifying the number of metagenomic reads that belong to them, and found that they significantly constitute less of the microbial community in the mice with SCI.
MC: Some of the changes were dependent on the level of injury. Why do you think this might be?
AZ: We think that the loss of sympathetic tone is the mechanism behind this. After SCI, normal sympathetic nervous system control over the small bowel and colon can be impaired, depending on where this injury happens. The higher the injury level along the spinal cord, the larger the loss of innervation to the gut, and the more severe the dysregulation of gut physiology.
MC: Are you able to highlight any limitations to the work?
AZ: Our current study was “pilot” in its nature. We had only 15 mice across the 3 groups examined. Hence, many additional interesting patterns that we were able to see in the data were not discussed in the publication due to the lack of statistical support behind these specific observations. We are currently working on rectifying this by including a larger number of mice in our study to examine if these further biological observations are supported or not.
MC: Why should the scientific community and general public know about this research?
AZ: Our study provides critical blueprints of the microbiome changes after spinal cord injury that are now made available to the spinal cord, the gut microbiome and more broadly the medical research communities. These blueprints are high resolution and provide gene- and genome-level information on both microbes and viruses. It also implies to the public that gut microbes are integral to our health, and that the impact of their metabolic activity might be important even in very severe diseases such as after SCI.
MC: What are your next steps in this space?
AZ: We are now working on investigating more of the biological changes that happen in the gut after spinal cord injury. We will work with more mice and introduce new analytical and bioinformatic tools to characterize the “beneficial/harmful” microbes and their viruses. These efforts may allow for targeted manipulation of the gut microbiome to decrease the severity of the symptoms associated with chronic conditions, such as those that happen after spinal cord injury.
Ahmed Zayer was speaking to Molly Campbell, Science Writer for Technology Networks.
Reference: Du Jingjie, Zayed Ahmed A., Kigerl Kristina A., et al. Spinal cord injury changes the structure and functional potential of gut bacterial and viral communities. mSystems. 0(0):e01356-20. doi:10.1128/mSystems.01356-20.


