Revolutionizing the Science of Nerve Repair and Regeneration
Complete the form below to unlock access to ALL audio articles.
Peripheral nerve damage is estimated to affect more than 20 million people in the United States, causing symptoms that range from mild discomfort to severe disability. Damage is often undiagnosed or untreated, and current standard of care procedures can be associated with limitations that impact quality of life. Axogen, a company focused on the science, development, and commercialization of technologies for peripheral nerve regeneration and repair, aims to address these issues and provide more efficient treatment options to patients.
To learn more about the causes and consequences of peripheral nerve damage and some of the solutions available to patients, Technology Networks spoke with Karen Zaderej, chief executive officer of Axogen.
Anna MacDonald (AM): What are the main causes and consequences of peripheral nerve damage?
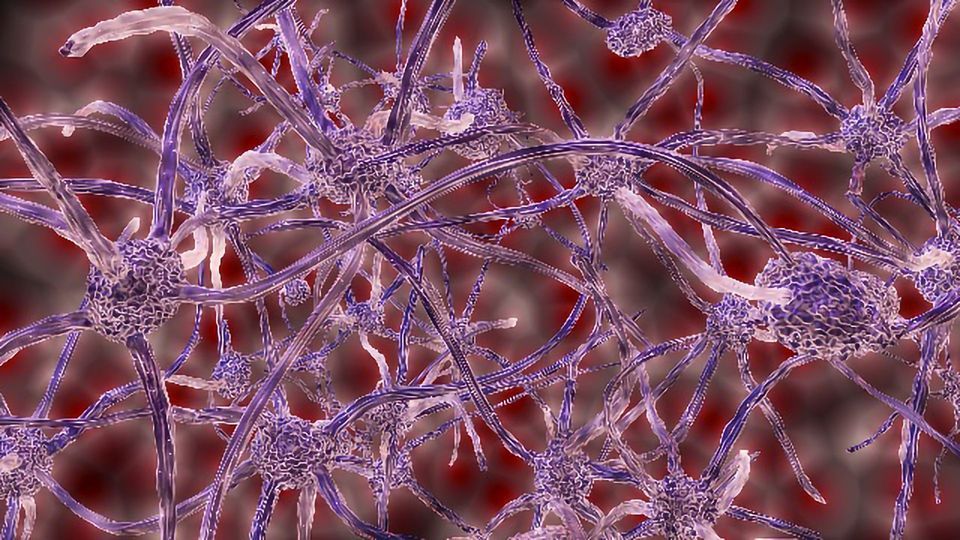
Karen Zaderej (KZ): Nerves are like electrical wires—they carry signals to and from your brain throughout your entire body. Nerves give you the ability to move, feel, touch and much more. When a nerve is cut or damaged, those signals are interrupted, which can cause pain, numbness, burning or loss of function in the affected area. Every day, people suffer traumatic injuries or undergo surgical procedures that impact the function of their peripheral nerves.
One of the leading causes of peripheral nerve damage is traumatic injury resulting from things like workplace injuries, sports injuries, kitchen mishaps, and other accidents like falls or cuts that often occur during day‐to‐day activities. Approximately 700,000 Americans undergo surgical procedures every year in which traumatic peripheral nerve damage may be repaired.
AM: Can you describe current standard‐of‐care procedures for peripheral nerve repair?
KZ: Many nerve injuries go undiagnosed and untreated. Often, people are unaware that the pain, loss of sensation or limited motor function that they are experiencing comes from peripheral nerve damage. Currently, many patients and surgeons accept the pain and functional loss as an inevitable outcome of surgery or injury. Damaged peripheral nerves can be surgically repaired, and if repaired properly, the nerves can regenerate. But the window of time for the best surgical outcome can be limited, so consulting a peripheral nerve specialist should be done quickly.
Current standard of care procedures focus on three types of nerve injuries. Transection, the most common form of traumatic nerve injury, occurs when peripheral nerves are severed. The current standard‐of‐care procedure for long‐gap injuries involves removing a nerve from another part of the patient’s body in order to repair the damaged nerve. This will likely cause a loss of sensation and may result in pain at the donor site.
The current standard‐of‐care procedure for small‐gap injuries is direct repair. This technique pulls the ends of the nerve together and holds them in place with suture. Depending on the anatomical location and the extent of the injury, this method may result in tension at the repair site, which can reduce blood flow within the nerve and inhibit proper nerve regeneration, resulting in impaired function and risk of pain. Synthetic conduits, introduced approximately 20 years ago, may provide an off‐the‐shelf option for bridging small‐gap nerve injuries.
Compression injury is a form of nerve damage resulting from constriction of the nerve and an overwhelming amount of pressure on nerves. This compression alters the signaling of the nerve and can cause muscle weakness, abnormal sensation, and pain. Current standard‐of care surgical procedures to relieve compression involve cutting away the tissue constricting the nerve and then covering the nerve to protect it using either vein, collagen wraps, or a piece of the body’s own fat.
Amputations, mastectomies, and previous surgeries can cause a third type of peripheral nerve damage known as stump neuromas. Stump neuromas are a tangle of nerve and scar tissue that forms when nerves are cut and left unrepaired. They are typically painful and easily irritated. Current standard‐of care procedures include traction neurectomy in which the nerve is stretched, the neuroma is cut off, then the nerve is allowed to retract into the surrounding tissue or burying the nerve end into muscle or bone after removal of the neuroma. Other treatment options include a chemical injection into the neuroma in an attempt to kill some of the nerve that is carrying the painful signal.
AM: How are Axogen’s nerve repair solutions different?
KZ: Axogen's platform for peripheral nerve repair features a comprehensive portfolio of products, including Avance® Nerve Graft, a biologically active off‐the‐shelf processed human nerve allograft for bridging severed peripheral nerves with gaps up to 70mm without the comorbidities associated with a second surgical site; Axoguard Nerve Connector®, a porcine submucosa extracellular matrix (ECM) coaptation aid for tensionless repair of severed peripheral nerves with gaps up to 5mm; Axoguard Nerve Protector®, a porcine submucosa ECM product used to wrap and protect damaged peripheral nerves and reinforce the nerve reconstruction while minimizing the potential for soft tissue attachments; and Axoguard Nerve Cap®, a chambered porcine submucosa ECM product used to protect a peripheral nerve end and separate the nerve from the surrounding environment to reduce the development of symptomatic or painful neuroma.
Avance Nerve Graft, our flagship product, revascularizes and remodels into a patient’s own nerve tissue, similar to an autologous nerve. Our proprietary process cleanses away cellular and noncellular debris while preserving the essential inherent structure of the nerve extracellular matrix (ECM). This off‐the‐shelf option eliminates the risk of comorbidities associated with the second surgical site often required for the traditional standard‐of‐care method.
One significant application of Avance Nerve Graft is during breast reconstruction after mastectomy. Most women who undergo a mastectomy experience partial to complete loss of sensation because nerves that are cut during the mastectomy are not reconnected during their reconstruction. Resensation®, is a new technique that incorporates breast neurotization, or nerve repair, into the reconstructive procedure. This can potentially restore feeling to the reconstructed breast. When sensation is restored to breasts after mastectomy and reconstruction, women have the ability to not only look, but also may feel, more like themselves again.
Another significant application of our technologies is in the treatment of chronic neuropathic pain. Pain is multi‐factorial, but for many patients it can be traced back to a damaged nerve. Though nerves naturally regrow and regenerate, when they’re damaged, they may not do so properly. As a result, a tangled mass of scar tissue called a neuroma can form, disrupting normal nerve function and potentially causing chronic pain. Often, the first course of action for patients with chronic pain is to manage the symptoms through pain medications, physical therapy or other noninvasive treatments. Many of these treatments offer temporary relief or cover up the symptoms, but do not fix the source of the pain. Surgical nerve repair focuses on identifying and repairing the cause of the pain, potentially providing a much more permanent solution. The physical causes of nerve pain can be a neuroma, compression of the nerve or both. If a neuroma is identified as the cause of the pain, a surgeon can locate and remove the neuroma. This gets rid of the painful stimulus and stops the pain signals to the brain. Then, a surgeon can repair the nerve by either reconnecting the nerve with an Avance Nerve Graft to allow restoration of normal signals to the brain, isolating the nerve end with a nerve cap such as Axoguard Nerve Cap to reduce the potential for neuroma formation, or occasionally rerouting the nerves. To repair nerve compression, your surgeon will need to release the traumatized tissue that’s pressing on or strangling the nerve. This is often done by cutting or removing the surrounding tissue that is causing the constriction. Releasing the tissue relieves the pressure placed on the nerve and allows it to regain mobility and appropriate circulation. The surgeon may decide to protect the nerve by placing fat around it, wrapping the nerve with vein tissue, or using an off‐the‐shelf protector such as the Axoguard Nerve Protector.
Axogen technologies are used by a wide variety of specialists such as reconstructive plastic surgeons, orthopedic and plastic hand surgeons, and oral and maxillofacial surgeons.
AM: What future advancements in nerve repair do you envision?
KZ: Given the vast network of peripheral nerves in the body, the opportunity to apply Axogen solutions to additional areas of nerve repair is substantial. We will continue investing in scientific research, clinical studies, and physician education, which have become the foundation of the company’s innovations. Axogen will continue to explore new nerve repair products and applications where we believe we can bring meaningful solutions to current clinical challenges.
Our technologies and techniques have been extensively evaluated by more than 400 surgeon and clinical investigators and results have been published in more than 150 peer‐reviewed clinical publications. These powerful clinical outcomes are made possible by partnerships between our purpose‐driven team, clinicians, and patients. Together, we are building the peripheral nerve repair market, expanding applications, and increasing adoption of our transformative technologies and techniques—all with the goal of addressing unmet patient needs and advancing a meaningful pipeline of nerve repair solutions.
Karen Zaderej was speaking to Anna MacDonald, Science Writer for Technology Networks.


