Mapping out Cell Conversion

Complete the form below to unlock access to ALL audio articles.
An international team of researchers from the Duke-NUS Medical School (Duke-NUS), the University of Bristol, Monash University and RIKEN have developed an algorithm that can predict the factors required to convert one human cell type to another. These game-changing findings have significant implications for regenerative medicine and lay the groundwork for further research into cell reprogramming.
It is known that cell types are not fixed, and that one cell type can be reprogrammed, or converted, to become another cell type by the addition of a unique set of cellular factors. This approach was brought to the fore by Shinya Yamanaka, whose Nobel prize-winning work involved the reprogramming of fibroblast cells from the skin to induced pluripotent stem cells (iPS). In theory, iPS could then be directly reprogrammed to become, for instance, retinal cells that could help treat macular or eye degeneration. In practice though, it seems there are technical and safety concerns with this approach of cell conversion due to the accumulation of cancerous mutations in the reprogrammed cells, therefore leading to unpredictable behaviour.
In addition, despite this breakthrough, determining the unique set of cellular factors that is needed to be manipulated for each cell conversion is a long and costly process that involved much trial and error. As a result, this first step of identifying the key set of cellular factors for cell conversion is the major obstacle researchers and doctors face in the field of cell reprogramming.
In order to overcome this obstacle, Duke-NUS Senior Research Fellow Dr Owen Rackham worked for five years to develop a computational algorithm to predict the cellular factors for cell conversions. The algorithm, called Mogrify(1), is able to predict the optimal set of cellular factors required for any given cell conversion.
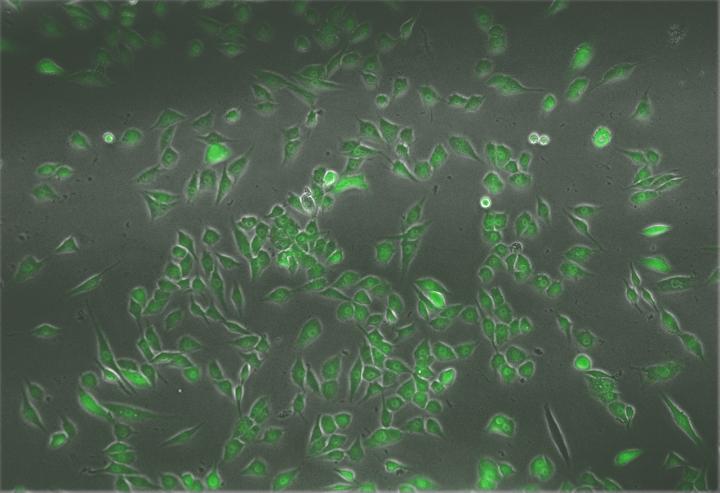
When tested, Mogrify was able to accurately predict the set of cellular factors required for previously published cell conversions correctly. To further validate Mogrify's predictive ability, the team conducted two novel cell conversions in the laboratory using human cells, and these were successful in both attempts solely using the predictions of Mogrify.
"Mogrify acts like a 'world atlas' for the cell and allows us to map out new territories in cell conversions in humans," explained Dr Rackham, who is from the Systems Genetics of Complex Disease Laboratory at Duke-NUS. "One of the first clinical applications that we hope to achieve with this innovative approach would be to reprogramme 'defective' cells from patients into 'functioning' healthy cells, without the intermediate iPS step. These then can be re-implanted into patients, and should, in practice, effectively enable new regenerative medicine techniques."
Associate Professor Enrico Petretto, co-author of the study and head of the Systems Genetics of Complex Disease Laboratory in the Centre for Computational Biology at Duke-NUS, highlighted that since Mogrify is completely data-driven, its robustness and accuracy can only continue to improve as more comprehensive data are collected and input into the framework.
"Mogrify is a game-changing method that leverages big-data and systems-biology; this will inspire new translational applications as the result of the work and expertise here at Duke-NUS," said Assoc Prof Petretto.
Mogrify has been made available online for other researchers and scientists. The team at Duke-NUS now plan to focus on Mogrify's application in translational medicine. Collaborative efforts between research groups within Duke-NUS are already in place to apply the algorithm to help develop treatments for specific diseases, such as cancer.



